Medicare Benefit, the private plan alternative to conventional Medicare, covers over half of eligible Medicare beneficiaries. Initially, one of many objectives of getting Medicare contract with non-public plans was to generate financial savings for the Medicare program by introducing competitors between non-public plans. Nonetheless, non-public plans have by no means generated financial savings for Medicare, partly as a result of the way in which Medicare pays non-public insurers has by no means sufficiently accounted for the variations in well being standing between beneficiaries in conventional Medicare and people enrolled in Medicare Benefit plans. As well as, the fee system was designed to draw insurers to the Medicare Benefit market, offering funds enough to keep up profitability in addition to to fund supplemental advantages, that are valued by enrollees. This has restricted the quantity of financial savings realized by the federal authorities when non-public plans obtain efficiencies and have decrease prices than conventional Medicare.
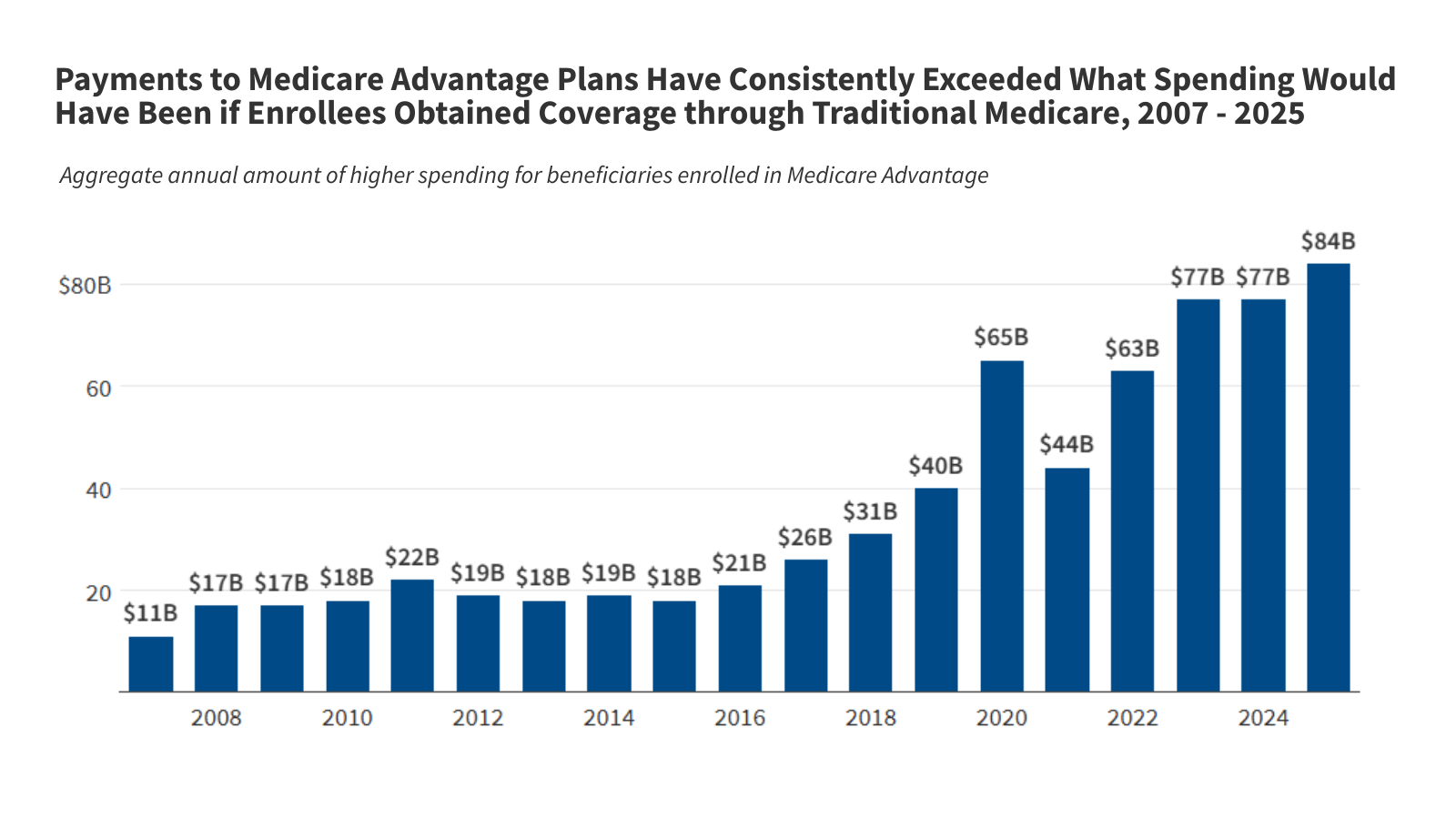
The Medicare Fee Advisory Fee (MedPAC) estimates that, in 2025, funds from the federal authorities to Medicare Benefit plans exceed what spending would have been in conventional Medicare by 20%, which interprets into $84 billion in extra spending. Larger funds to Medicare Benefit plans improve whole Medicare spending, pressure the Half A Hospital Insurance coverage belief fund and drive-up Half B premiums for all Medicare beneficiaries. This raises questions on whether or not the present fee system offers strong financial returns to insurers on the expense of the federal finances, Medicare beneficiaries themselves, and U.S. taxpayers, whereas additionally offering fashionable supplemental advantages similar to dental and imaginative and prescient for Medicare Benefit enrollees. It additionally raises questions on whether or not the present fee system ends in an inequitable distribution of supplemental advantages, in that it funds these extra advantages for Medicare Benefit enrollees however not conventional Medicare beneficiaries.
In response to press reports, some Senators briefly thought-about together with modifications to how the federal authorities adjusts funds to Medicare Benefit plans based mostly on the well being standing of their enrollees as a part of the reconciliation laws enacted into legislation on July 4, 2025. Some reportedly raised the opportunity of together with the No UPCODE Act, a bipartisan invoice that features a subset of fee reforms recommended by MedPAC. Whereas these modifications had been in the end not included within the reconciliation invoice, there seems to be ongoing curiosity in refining the present methodology for setting funds to plans, given the affect of the present fee system on Medicare spending and the federal finances.
This transient explains how Medicare Benefit funds are decided, together with an outline of the parameters which can be set in legislation and people that may be modified by the manager department by means of its regulatory authority. It additionally offers an summary of coverage choices to alter the Medicare Benefit fee system and features a glossary of phrases (italicized and bolded in textual content) associated to Medicare Benefit fee coverage.
Medicare Benefit funds are decided by means of an annual course of.
Personal plans have an extended historical past within the Medicare program, and the main points of how they’re paid have modified over time to deal with evolving coverage objectives, largely as a part of main items of laws, together with the Tax Fairness and Fiscal Duty Act of 1982 (TEFRA), the Balanced Price range Act of 1997, the Medicare Modernization Act of 2003, and the Inexpensive Care Act of 2010 (ACA).
Medicare Benefit plans obtain a month-to-month fee per enrollee from the federal authorities to supply Medicare-covered companies. Typically, the funds obtained from the federal authorities are enough for plans to additionally cowl supplemental advantages, similar to imaginative and prescient, listening to, and dental companies, to scale back value sharing in contrast to what’s required beneath conventional Medicare and not using a complement, and to buy-down the Half D premium for plans that supply prescription drug protection. Congress established the framework for the Medicare Benefit fee system giving the Secretary of the Division of Well being and Human Companies (HHS) authority in how it’s carried out. In every step of the annual fee course of described beneath, some elements are set in statute (lots of which had been considerably revised by the ACA), whereas the Secretary of HHS is directed to outline others, which is carried out by the Facilities for Medicare & Medicaid Companies (CMS), the federal company that oversees and administers the Medicare program.
Benchmarks are the utmost quantity the federal authorities can pay Medicare Benefit plans.
The utmost quantity the federal authorities can pay non-public insurers in a county for a median beneficiary who enrolls in a plan is named the benchmark. This quantity is a share of what the federal authorities spends on beneficiaries in conventional Medicare within the county. The legislation stipulates that every one counties nationwide are to be divided into quartiles based mostly on conventional Medicare spending and units the benchmark as a selected share. The utmost quantity the federal authorities can pay non-public plans is lower than conventional Medicare in one-quarter of counties and is the same as or greater than conventional Medicare within the different three-quarters of counties.
Particularly, counties within the first quartile with the best spending (similar to Miami-Dade County, Florida) have a benchmark set at 95% of conventional Medicare spending. Counties within the second and third quartiles have benchmarks set at 100% and 107.5% of conventional Medicare spending, respectively. And counties within the fourth quartile with the bottom spending (similar to Hennepin County (Minneapolis), Minnesota) have a benchmark of 115% of conventional Medicare spending.
The legislation additionally states that benchmarks are to be elevated by a certain quantity for plans that obtain not less than a 4-star ranking beneath the high quality bonus program. In most counties, benchmarks are elevated by 5 share factors for qualifying plans. The rise is 10 share factors for qualifying plans in city counties with traditionally excessive Medicare Benefit penetration and with lower-than-average conventional Medicare spending (double bonus counties). Benchmarks are capped and can’t be increased than they might have been previous to the ACA.
In every U.S. county, the calculation of conventional Medicare spending for setting the benchmark consists of spending for beneficiaries with Elements A and B, and beneficiaries with Half A solely or Half B solely, despite the fact that enrollment in each Half A and Half B is required for Medicare Benefit. Together with Half A solely and Half B solely beneficiaries within the calculation of conventional Medicare spending for the aim of calculating benchmarks has the impact of lowering common conventional Medicare spending in comparison with what it could be if spending was based mostly solely on beneficiaries enrolled in each Half A and Half B.
Whereas the legislation broadly defines find out how to take into account historic conventional Medicare spending for functions of setting Medicare Benefit benchmarks, it directs the Secretary of HHS, by means of CMS, to compute the per capita fee for funds and publish this quantity. CMS, subsequently, decides find out how to incorporate out there information, in addition to the financial and different assumptions to make use of when forecasting how well being care spending will develop (since CMS is setting the fee for the upcoming 12 months). CMS additionally develops, revises, administers and evaluates the strategies used to calculate and assign star rankings, that are used to find out the annual will increase within the benchmarks, in addition to rebates obtained by plans (described beneath), and can be found for beneficiaries to make use of to check plans. To derive star rankings, CMS determines the particular high quality measures to make use of, the supply and 12 months of knowledge, find out how to weight measures, and the lower factors for particular star values. In October of every 12 months, CMS publishes updates to high quality star rankings, which seem on the Medicare Plan Finder and are used for the next fee 12 months (after the one starting within the coming January). That’s, the standard star rankings revealed within the fall of 2025 shall be used to find out funds for plans out there to beneficiaries in 2027.
CMS publishes an Advance Discover of proposed methodological modifications and fee insurance policies early within the calendar 12 months and a remaining Charge Announcement, together with the county-level benchmarks, by the primary Monday in April. Together with the speed announcement, CMS makes the fee guide, as well as the bid pricing instrument out there presently. This offers plans the data and time wanted to organize their bids (described within the subsequent part).
Insurers submit bids to cowl Medicare A and B companies.
After CMS publishes the ultimate fee announcement, insurers estimate how a lot it’s going to value to cowl Medicare Half A and Half B companies (excluding hospice) for the common Medicare beneficiary beneath every Medicare Benefit plan they suggest to supply, plus administrative bills and revenue. Insurers submit their bids to CMS by the primary Monday in June. (There may be an exception to this course of for employer- and union- sponsored plans, which don’t submit bids, and as a substitute are assigned a bid quantity based mostly on the enrollment-weighted common of bids for plans out there in the identical counties.) CMS is liable for reviewing, negotiating, and in the end figuring out whether or not to simply accept a bid. CMS publishes the accredited Medicare Benefit plans forward of the October 1st launch of the advertising interval for the approaching 12 months and Medicare’s annual open enrollment interval that runs from October 15 by means of December 7.
The legislation requires insurers to submit sure info as a part of their bid, together with: an outline of the proposed prices of offering all objects and companies lined beneath the plan, the proportion attributable to Medicare-covered Half A and Half B advantages, fundamental Half D prescription drug protection, and supplemental advantages. Plans are additionally required to submit the actuarial foundation used of their calculations, together with an outline and the actuarial worth of deductibles, coinsurance, and copayments. Plans are required to spend not less than 85% of their income on plan-covered companies (together with further advantages), leaving 15% for administrative bills and revenue. That is additionally known as the medical loss ratio (MLR). Further directions to insurers, together with info that CMS requires as a part of the bid are addressed within the Annual Charge Announcement and included within the directions for the bid pricing instrument.
Funds to Medicare Benefit plans are comprised of two elements, the bottom fee and the rebate.
For all accredited bids, CMS calculates how a lot the federal authorities can pay the Medicare Benefit plan per enrollee, by evaluating the insurer’s bid (to cowl the price of offering Medicare Half A and Half B companies) to the benchmark. The exact benchmark towards which a bid is in contrast is dependent upon whether or not the plan is a neighborhood or regional plan, and the particular counties during which the plan operates. Bids for plans that function throughout a number of counties are in contrast towards a weighted common benchmark constructed utilizing projections for plan enrollment throughout the totally different counties.
The funds to Medicare Benefit plans embody the next two elements:
- Base fee. For plans that bid at or beneath the benchmark, the bottom fee is 100% of the plan’s bid. If the bid is above the benchmark, the plan’s base fee is the same as the benchmark quantity, and enrollees in that plan pay a supplemental premium equal to the distinction between the bid and the benchmark.
- Rebate. Along with the bottom fee, plans that bid beneath the benchmark obtain a portion of the distinction between the benchmark and bid, which is named a rebate. (Plans that bid at or above the benchmark obtain no rebate.) The share of the distinction a plan will get is dependent upon the standard star ranking of the contract of which it’s a half (most Medicare Benefit contracts embody a number of plans) and is laid out in legislation. The rebate share is 70% of the distinction for plans which can be a part of contracts with not less than 4.5 stars, 65% for plans which can be a part of contracts with 3.5 to 4.5 stars, and 50% for plans which can be a part of contracts with lower than 3.5 stars.
- Plans are required by legislation to make use of the rebate {dollars} to scale back value sharing, pay for non-Medicare lined advantages (for instance, dental, imaginative and prescient, and listening to companies), or scale back the Half B and/or Half D premium (in addition to to cowl related administrative prices and revenue). Since 2018, the rebate portion of the fee has almost doubled for particular person plans, that are broadly out there for common enrollment, and greater than doubled for particular wants plans, that are plans that prohibit enrollment to beneficiaries with particular care wants or who’re dually eligible for Medicare and Medicaid (Determine 1). Virtually all Medicare Benefit plans now present supplemental advantages, often for no extra premium.
Funds to Medicare Benefit plans are adjusted for the well being standing of enrollees.
The legislation requires CMS to regulate funds to Medicare Benefit plans for sure demographic traits and the well being standing of enrollees. That is known as threat adjustment, and beneath this course of enrollees are assigned a threat rating that’s supposed to function a predictor of their anticipated well being care spending. CMS is liable for creating the threat adjustment mannequin, together with deciding which information to make use of, the variety of years of prognosis information to include, and the set of diagnoses that can issue into the danger rating.
CMS periodically revises and updates the danger adjustment mannequin, together with how it’s referenced (i.e., shifting from V24 to V28, the present model in use) and offers notification within the Advance Discover when it proposes to make modifications. For instance, this occurred in 2023 when CMS proposed an replace to the information used to calibrate the danger adjustment mannequin and the 12 months used to estimate the impact of the various factors within the mannequin, in addition to modifications to how sure circumstances that had been coded extra ceaselessly in Medicare Benefit than in conventional Medicare had been integrated (or not) into the danger adjustment mannequin. After contemplating feedback on their proposed modifications, together with from industry representatives that had been involved in regards to the affect on advantages and prices, modifications had been incorporated into V28 and adopted by means of a phased in course of throughout plan years 2024 and 2025. CMS additionally makes selections about different mannequin specs, similar to find out how to scale threat scores in order that the common rating for conventional Medicare beneficiaries within the fee 12 months is the same as 1 (that is known as the normalization issue).
The legislation requires the Secretary to scale back Medicare Benefit threat scores by not lower than 5.9 % to account for the distinction in coding patterns between Medicare Benefit and conventional Medicare if the danger mannequin is developed utilizing conventional Medicare information (which it presently is). The requirement for an automated discount in threat scores is as a result of Medicare Benefit enrollees are inclined to have extra documented diagnoses than they might if lined beneath conventional Medicare. (See subsequent part for a fuller dialogue of coding depth.)
Medicare Benefit funds exceed anticipated spending in conventional Medicare.
Medicare funds to Medicare Benefit insurers constantly exceed the quantity Medicare would have been anticipated to spend on enrollees in the event that they had been lined beneath conventional Medicare, in line with MedPAC (Determine 3). In 2025, MedPAC estimates that funds per enrollee are 20% increased than anticipated spending could be in conventional Medicare. That interprets into $84 billion of extra spending for 2025 alone. The upper funds to plans and the related increased spending beneath Medicare may be attributed nearly totally to coding depth ($40 billion) and favorable choice ($44 billion), described in additional element beneath.
Coding depth contributes to increased spending for Medicare Benefit enrollees.
The present threat adjustment system depends on diagnoses from well being care encounters within the prior 12 months and usually offers increased funds to Medicare Benefit plans for enrollees with extra reported diagnoses. This technique creates incentives for Medicare Benefit plans to doc extra well being circumstances for his or her enrollees than would have been recorded in conventional Medicare. In conventional Medicare, well being care suppliers solely should document sufficient details about an individual’s identified well being care circumstances to help the service for which fee is being submitted. This ends in Medicare Benefit enrollees trying sicker than they might if they’d been lined beneath conventional Medicare. For the reason that threat adjustment mannequin is calibrated on conventional Medicare beneficiaries, the distinction in coding practices implies that the mannequin overpredicts spending for Medicare Benefit enrollees and thus pays extra for Medicare Benefit enrollees than if they’d been lined beneath conventional Medicare. MedPAC estimates that increased coding depth in Medicare Benefit contributes $40 billion of the $84 billion in extra Medicare spending in 2025.
Medicare Benefit insurers make the most of instruments which can be by no means or hardly ever utilized in conventional Medicare to seize extra diagnoses than are included on well being care claims, similar to chart evaluations and well being threat assessments (HRAs), a few of which happen in an individual’s residence relatively than in a medical setting. On the one hand, capturing extra diagnoses might assist Medicare Benefit organizations higher handle look after enrollees by offering a extra full image of somebody’s well being. However alternatively, such coding practices improve funds to Medicare Benefit insurers typically with out bettering care. Analyses by the Health and Human Services Office of the Inspector General (HHS OIG) and Wall Street Journal discovered, for instance, that enrollees in Medicare Benefit plans ceaselessly had no well being care companies related to most of the diagnoses that seem in submissions used to calculate threat scores. MedPAC estimates that in 2023, diagnoses documented from chart evaluations and HRAs contributed $24 billion and $15 billion, respectively, to whole Medicare Benefit spending, a discovering in step with estimates by different researchers.
The extent to which the embedded incentives and use of extra instruments impacts threat scores varies substantially throughout Medicare Benefit insurers. MedPAC discovered that in 2023, 85% of Medicare Benefit enrollees had been in a plan sponsored by an insurer estimated to have coding practices that elevated their enrollees’ threat scores by greater than CMS’ 5.9% discount in threat scores. In different phrases, even with the across-the-board 5.9% discount to threat scores utilized by CMS, funds for the overwhelming majority Medicare Benefit enrollees stay increased than anticipated spending in conventional Medicare resulting from coding depth.
The reporting of diagnoses for threat adjustment that aren’t supported by an individual’s medical document might be resulting from inadequate documentation or probably represent fraud. Threat Adjustment Information Validation (RADV) audits are the first instrument the federal government makes use of to determine and recuperate funds to plans that had been made based mostly on such diagnoses. Nonetheless, resulting from restricted sources and workers at CMS allotted for RADV audits, the federal authorities has audited solely a small share of Medicare Benefit contracts and has not recouped a considerable quantity of Medicare funds made to plans based mostly on coding practices that might not be justified.
In Could 2025, CMS beneath the Trump administration announced it could audit each Medicare Benefit contract each fee 12 months, considerably improve the workers devoted to finishing up these audits, and expedite the completion of audits launched between 2018 and 2024. Nonetheless, it’s not clear whether or not CMS has taken any steps to rent the brand new workers. Moreover, a federal decide not too long ago struck down a rule finalized beneath the Biden administration associated to RADV audits, which can additional complicate CMS’ skill to implement its introduced audit technique. However, Dr. Mehmet Oz, the present Administrator for CMS, continues to express concern about coding practices that doc extra circumstances with out accompanying remedy, suggesting it will stay a precedence for the company. The Department of Justice additionally has a number of ongoing instances alleging that sure insurers submitted diagnoses to CMS for threat adjustment functions that aren’t legitimate, that means the enrollee doesn’t have the situation in any respect, and thus are unlawful beneath the False Claims Act.
Favorable choice into Medicare Benefit plans additionally results in increased Medicare spending.
Amongst individuals with the very same threat rating (based mostly on reported diagnoses and different traits) that’s used to estimate anticipated well being care spending, precise spending will differ. In different phrases, some individuals use extra companies and incur considerably increased prices than others who’ve the identical reported medical circumstances. If individuals whose precise spending is decrease than common amongst all individuals with the identical threat rating usually tend to enroll in Medicare Benefit, then there may be favorable choice into Medicare Benefit as a result of the precise value of offering protection for enrollees (earlier than any results from care administration) is decrease than the funds made to plans. Evaluation evaluating conventional Medicare spending amongst individuals who subsequently enroll in Medicare Benefit and people who stay in conventional Medicare implies favorable choice as a result of conventional Medicare spending amongst beneficiaries with comparable threat scores was lower for individuals who subsequently enrolled in Medicare Benefit than beneficiaries who stayed in conventional Medicare. MedPAC estimates that favorable choice contributes $44 billion of the $84 billion in extra Medicare spending in 2025.
One cause spending varies throughout individuals with the identical threat rating is that people who find themselves the identical age and intercourse with the identical well being circumstances (the first inputs into the danger rating mannequin) differ in how a lot well being care they really use, even when their predicted spending could be the identical based mostly on having the identical threat rating. Many issues that have an effect on an individual’s use of well being care companies will not be captured within the threat rating mannequin, together with private preferences or circumstances, tolerance for threat, or medical nuances that require kind of administration of a selected situation.
Within the presence of utilization administration instruments which can be widespread options of Medicare Benefit plans, similar to prior authorization, referral necessities, and the usage of networks, individuals who anticipate to make use of extra well being care companies might favor to obtain their protection from conventional Medicare, the place these instruments are usually not used. Whereas these utilization administration instruments might deter use of pointless or clinically inappropriate companies and scale back what the plan spends on Medicare-covered companies, these results are separate from the affect of favorable choice.
Efficiencies achieved by Medicare Benefit insurers don’t assure financial savings for the federal authorities.
Even with out the variations in spending resulting from coding depth and favorable choice, when plans function effectively and have decrease prices than conventional Medicare, Medicare funds might nonetheless be increased for beneficiaries enrolled in Medicare Benefit plans than anticipated prices for these beneficiaries beneath conventional Medicare. It is because the fee system is just not designed for the federal authorities to retain nearly all of financial savings achieved by Medicare Benefit insurers.
First, benchmarks are set at or above conventional Medicare spending in three-quarters of counties (representing almost 60% of all Medicare beneficiaries), that means financial savings will not be assured in these counties as a result of the utmost quantity the federal authorities is prepared to pay is not less than as a lot as what spending could be in conventional Medicare. Second, benchmarks are additional elevated beneath the standard bonus program. For instance, in 2025, 75% of Medicare Benefit enrollees are in a plan that receives bonus funds, at an estimated value of not less than $12.7 billion in line with a previous KFF evaluation. Third, insurers’ rebate funds are set in order that they’re paid between 50% and 70% of the distinction between the benchmark and their bid (the estimated value of offering Medicare-covered companies), which limits the share of any financial savings attributable to efficiencies which can be retained by the federal authorities.
Whereas most Medicare Benefit plans estimate that their prices for masking Half A and Half B companies are nicely beneath conventional Medicare spending, with the common bid equal to about 83% of conventional Medicare spending, funds from CMS can nonetheless exceed spending in conventional Medicare, notably in counties with benchmarks set above conventional Medicare prices. That decrease spending might stem from plenty of elements, similar to lower use of well being care companies, together with fewer hospital admissions and fewer use of post-acute care.
Contemplate an illustrative county with a benchmark that’s 115% of conventional Medicare spending and common conventional Medicare spending of $1,000 per 30 days. Plans with a median bid and not less than a 4-star high quality ranking would probably obtain funds in extra of conventional Medicare spending. As proven in Determine 4, a 4-star plan with estimated prices which can be 17% beneath conventional Medicare spending, that may be a bid of $830, would obtain $1,071 a month for a median enrollee, in comparison with conventional Medicare spending of $1,000 per 30 days. On this instance, solely the 3-star plan would obtain modest ($10 per 30 days) financial savings for conventional Medicare.
Virtually all Medicare Benefit enrollees are in a plan that provides lowered value sharing and protection of non-Medicare lined companies, similar to dental, imaginative and prescient and listening to, often for no extra premium. Plans pay for these advantages utilizing their rebate {dollars}. Moreover, most individuals in a plan that features Half D prescription drug protection wouldn’t have to pay the Half D premium, as a result of the plan makes use of its rebate {dollars} to cowl this value. Thus, the upper funds to Medicare Benefit plans in comparison with spending in conventional Medicare permit non-public plans to supply extra advantages that enrollees probably worth. It’s tough to estimate how a lot worth enrollees get, nevertheless, as a result of detailed information on out-of-pocket spending, the usage of further advantages by enrollees, and plan spending by kind of additional profit are not readily available.
A wide range of proposals have been put ahead to reform the Medicare Benefit fee system.
The upper spending in Medicare Benefit relative to conventional Medicare has prompted quite a few proposals to reform the Medicare Benefit fee system. Some proposals purpose to deal with considerations associated to coding depth, both straight or by means of refinements to the methodology for adjusting funds to plans for the well being standing of enrollees (threat adjustment). Further proposals would modify particular levers within the present fee system, such because the methodology for figuring out benchmarks, the standard bonus program and star rankings, or introducing a brand new reinsurance program. And others would undertake extra basic modifications to the fee method, like implementing aggressive bidding for Medicare Benefit plans. Typically, proposals incorporate a number of reforms (Desk 1). In lots of instances, the proposals described on this part would require Congressional motion, whereas others might be carried out by CMS as a part of rulemaking or the annual fee announcement.
Adjustments to the Medicare Benefit fee system that lead to decrease funds to plans elevate considerations in regards to the affect on plan availability, advantages, and prices. Particularly, since plans use funds from the federal authorities to scale back value sharing, pay for non-Medicare lined companies, and purchase down the Half B and/or Half D premiums, some within the trade have argued that decrease funds will translate into fewer further advantages and better premiums and different prices for enrollees. Analysis of how Medicare Benefit insurers reply to fee modifications so far means that the results have been modest and that insurers have prioritized reducing their profits or lowering administrative costs over main modifications to fashionable advantages. Following modifications to the danger adjustment mannequin that had been phased in starting in 2024, some insurers lowered the variety of plans they supplied, although total the market was relatively stable. Finally, the response of insurers to modifications in fee, and the affect on beneficiaries, will depend upon the magnitude of the fee reductions and the way steadily the modifications are phased in time beyond regulation.
Proposals associated to coding depth and threat adjustment.
A number of choices to scale back the affect of coding depth variations between Medicare Benefit and conventional Medicare have been proposed. For instance, MedPAC recommends a number of coverage modifications, together with creating a threat adjustment mannequin that makes use of two years of conventional Medicare and Medicare Benefit diagnostic information to scale back year-to-year variation within the documentation of diagnoses, excluding diagnoses from HRAs (in both conventional Medicare or Medicare Benefit), and making use of a coding adjustment that absolutely accounts for any remaining variations between conventional Medicare and Medicare Benefit. The Congressional Price range Workplace (CBO) has estimated {that a} subset of those insurance policies (utilizing two years of knowledge and excluding diagnoses from HRAs) would save $124 billion over 10 years (2025 – 2034).
Lately, insurance policies to deal with coding depth have additionally gotten elevated consideration from Congress. For instance, the No UPCODE Act, sponsored by Senator Invoice Cassidy (R-LA) and Senator Jeff Merkley (D-OR), largely modeled after the suggestions from MedPAC, would require CMS to exclude diagnoses from chart evaluations and HRAs, use two years of diagnostic information, and have in mind variations in Medicare Benefit and conventional Medicare coding patterns when figuring out changes to Medicare Benefit fee. The laws has been launched in two successive classes of Congress.
Some proposals would improve the coding depth adjustment utilized to all Medicare Benefit plans above the 5.9% minimal. CBO included two variations of a rise within the across-the-board adjustment in its most up-to-date set of Choices for Lowering the Deficit, estimating that over 10 years, increasing the across-the-board risk score reduction from 5.9% to 8% would save $159 billion, while an increase from 5.9% to 20% would save more than $1 trillion (both over the 2025 – 2034 time period). A modification of this option would apply a tiered adjustment based on plans’ historical coding behaviors, so plans with higher coding intensity would have a higher adjustment. (CBO has not released an estimate of savings from this option.)
Proposals related to benchmarks.
Options to revise how the federal government determines benchmarks for Medicare Advantage payments include both changes to the quartile system and changes to the calculation of spending in traditional Medicare that serves as the basis for benchmarks. For example, MedPAC recommends changing the present method to benchmarks (based mostly on conventional Medicare spending in counties, stratified by quartiles) with a coverage that blends native space conventional Medicare spending with standardized nationwide conventional Medicare spending. This method would preserve benchmarks above conventional Medicare spending in low-spending areas, sustaining incentives for insurers to take part in these markets, and beneath conventional Medicare spending in high-spending areas, permitting the Medicare program to scale back total spending. The method additionally goals to deal with considerations about basing benchmarks on conventional Medicare spending in counties with very excessive Medicare Benefit penetration and smooths the variations throughout counties with comparable conventional Medicare spending. The proposal would additionally apply a 2% low cost fee to the benchmark to make sure the federal authorities retains a minimal degree of financial savings. A few of the financial savings achieved by the MedPAC proposal could be offset by its suggestion to calculate conventional Medicare spending based mostly on beneficiaries enrolled in each Medicare Half A and Half B (relatively than embody beneficiaries with Half A solely or Half B solely), which has a considerable value, and by eliminating the coverage that caps benchmarks at their pre-ACA degree. Below this suggestion, the rebate share could be set at 75% for all plans (relatively than tied to star rankings). In June 2021, MedPAC estimated that taken altogether, these modifications would lead to $10 billion in financial savings over 5 years.
Different variations of choices to revise the benchmark system embody capping benchmarks at a % of conventional Medicare prices or imposing necessities that changes to the benchmark scale back mixture funds in order that they do not exceed spending for comparable beneficiaries in conventional Medicare. Paragon Health Institute estimates that capping benchmarks at 100% of conventional Medicare spending in all counties besides these with the bottom Medicare Benefit penetration would save $385 billion over 10 years.
Proposals associated to high quality bonus program and star rankings.
Proposals to reform the Medicare Benefit program typically embody replacing, modifying, or ending the standard bonus program, and revising the standard star rankings system on which bonuses are based mostly. For instance, one Congressional proposal would finish the benchmark will increase for plans that get hold of sure high quality scores. As well as, MedPAC has proposed a complete reform to the standard ranking system that might change the standard bonus program with a Medicare Benefit Worth Incentive Program (MA-VIP). The MA-VIP would rating a small set of measures, consider high quality on the native degree, account for social threat elements, distribute rewards based mostly on a steady scale so that there’s not a pointy “cliff” the place solely plans above a sure threshold get a bonus, and incorporate each rewards for higher-performing plans and penalties for lower-performing plans. In June 2020, MedPAC estimated that these modifications would save greater than $10 billion over 5 years.
An alternative choice consists of making the standard bonus program finances impartial by offsetting spending on bonuses for high-quality plans with penalties paid by low-quality plans. The Committee for a Responsible Federal Budget (CRFB) estimates that making the standard bonus program finances impartial would save between $115 billion and $170 billion over 10 years (2024 – 2033).
Moreover, a narrower method that largely retains the standard bonus program however eliminates double bonus counties would produce some financial savings. CBO estimates that eliminating double bonuses would save $18 billion over 10 years (2019 – 2028), however that financial savings estimate might be bigger now given the expansion in Medicare Benefit enrollment because the estimate was developed.
Proposals associated to reinsurance or stop-loss funds.
One other method would establish a reinsurance mechanism to guard Medicare Benefit insurers from extraordinarily excessive and surprising prices that aren’t in any other case addressed by the danger adjustment mannequin. For instance, insurers might be paid extra for enrollees that had spending that was considerably increased than predicted, whereas insurers with enrollees with considerably decrease than predicted spending would make funds into this system, designed so the entire system was finances impartial (often called a two-sided method). One Congressional proposal consists of stop-loss funds for plans that have considerably increased expenditures than anticipated and authorizes the Secretary to implement such funds in a budget-neutral method.
Aggressive bidding proposals.
An alternative choice would shift away from conventional Medicare spending as the idea for benchmarks and as a substitute use bids submitted by insurers that estimate the price of offering Half A and Half B companies to find out the benchmark. This method is known as aggressive bidding. For instance, beneath this method, the utmost Medicare fee to plans (benchmarks) might be set on the enrollment-weighted average of bids submitted to supply a typical profit bundle, just like the method used within the Half D fee system. CBO has not scored a aggressive bidding method in recent times. The Bipartisan Policy Center estimates that this modification might save between $400 billion and $500 billion over 10 years (2024 – 2033).
| Desk 1 | ||
| Proposals to Reform the Medicare Benefit Fee System | ||
| Class Abstract | Examples | Financial savings Estimates |
| Coding Depth and Threat Adjustment: Cut back the affect of coding depth variations between Medicare Benefit and conventional Medicare. | Exclude diagnoses from HRAs from threat adjustment mannequin (MedPAC, No UPCODE Act, H.R. 3467)
Exclude diagnoses from chart evaluations from threat adjustment mannequin (No UPCODE Act, H.R. 3467) Use two years of knowledge (MedPAC, No UPCODE Act, H.R. 3467) |
Use two years of knowledge in threat mannequin and make diagnoses from HRAs ineligible for threat adjustment: $124B (CBO, 2025-2034) |
| Benchmarks: Transfer away from the quartile system and revise calculation of conventional Medicare spending. | Use a mix of nationwide and native conventional Medicare spending (MedPAC)
Use spending for conventional Medicare beneficiaries enrolled in each Half A and Half B (MedPAC, Paragon Well being Institute) Eradicate benchmark cap based mostly on pre-ACA spending (MedPAC, Paragon Well being Institute) Low cost benchmark by 2% (MedPAC) Cap benchmarks at 100% of conventional Medicare spending, besides in counties with low Medicare Benefit penetration (Paragon Well being Institute) |
Mixing nationwide and native conventional Medicare spending: $10B over 5 years (MedPAC, est. in 2021) Capping benchmarks at 100% of conventional Medicare spending: $385B (Paragon Well being Institute, est. in 2024) |
| High quality Bonus Program and Star Scores: Exchange, modify, or finish high quality bonus program and/or revise star ranking system. | Make high quality bonus program finances impartial (CFRB) Finish benchmark will increase for plans that get hold of sure high quality scores (H.R. 3467) Eradicate double bonus counties |
Eliminating double bonuses: $18.2B (CBO, 2019-2028) Making QBP finances impartial: $115-170B (CFRB, 2024-2033) |
| Reinsurance or Cease Loss: Set up mechanism to guard insurers from extraordinarily excessive and surprising prices. | Cease-loss funds to plans that have considerably increased spending than anticipated (H.R.3467) | Price range impartial |
| Aggressive Bidding: Use plan estimates of prices to cowl commonplace set of advantages to set benchmark. | Set benchmark on the enrollment-weighted common of Medicare Benefit insurer bids to supply a standardized profit bundle (Schaeffer Initiative for Well being Coverage, Bipartisan Coverage Middle) | Benchmark set to enrollment-weighted common of bids: $400B to $500B (BPC, 2024-2033). |
This work was supported partly by Arnold Ventures. KFF maintains full editorial management over all of its coverage evaluation, polling, and journalism actions.