This transient was up to date on October 7, 2025 to replicate provisions within the tax and spending bill enacted in July 2025, in addition to an outline of proposed modifications within the 2026 Medicare Doctor Price Schedule proposed rule issued on July 14, 2025.
Greater than 67 million folks—20% of the U.S. population—obtain their medical health insurance protection by the federal Medicare program. Among the many mostly used providers that Medicare covers are doctor providers and different outpatient providers coated below Medicare Half B. In 2021, 9 out of 10 beneficiaries in conventional Medicare used doctor and different Half B medical providers. Nearly half of the $1 trillion in gross Medicare profit spending in 2023 (49% or $493 billion) was spent on Half B providers. Medicare Half B spending accounts for 25% of all national spending for doctor and scientific providers.
Annually, the Facilities for Medicare & Medicaid Providers (CMS) updates Medicare funds for doctor providers and different Half B providers by rulemaking, based mostly on parameters established below legislation. In November 2024, CMS finalized a 2.83% decrease within the physician fee schedule conversion issue, a key facet of doctor cost charges below the Medicare program. This resulted in a median cost minimize of two.93% to physicians and different clinicians, which took impact on January 1, 2025 and stays in impact at this time. Congress thought-about however didn’t enact laws to reverse the minimize in Medicare doctor funds in a December 2024 spending bill and within the continuing resolution that funded the federal government by the top of the 2025 fiscal yr. The tax and spending invoice enacted in July 2025 provides for a one-time 2.5% enhance to doctor cost charges from January 1, 2026 by December 31, 2026, however doesn’t retroactively modify funds to compensate for the 2025 cost minimize.
Over time, physician groups and some policymakers have raised considerations that frequent annual cuts to Medicare doctor cost charges might push physicians to decide out of the Medicare program, creating potential entry issues for Medicare beneficiaries. Whereas virtually all non-pediatric physicians presently take part in Medicare, these considerations are a part of a broader discussion of potential reforms to Medicare doctor funds, which have additionally centered on points such because the long-standing gap in compensation between main care and specialty clinicians, the efficacy of quality-based cost incentives below the Quality Payment Program (QPP), and the affect of medical specialty teams and pursuits by the American Medical Affiliation (AMA)/Specialty Society Relative Worth Scale (RVS) Replace Committee (RUC), which issues annual recommendations to CMS on relative cost charges on the service stage. Notably, Robert Kennedy Jr., the Trump administration’s Secretary for the Division of Well being and Human Providers (HHS), has been critical of the RUC and has expressed ongoing curiosity in reducing its influence over cost charges.
In July 2025, CMS proposed updates to Medicare doctor funds for 2026 as a part of its annual rulemaking course of. These embody proposed changes to doctor cost charges in 2026, on prime of the rise within the tax and spending invoice famous above, in addition to a number of different potential modifications associated to doctor charges. Notably, it could modify the methodology used to calculate relative cost charges on the service stage, citing considerations concerning the accuracy and representativeness of survey information supplied by the AMA and the RUC, which have traditionally knowledgeable these calculations. The proposed rule additionally consists of measures to advertise extra versatile protection of telehealth providers, constrain spending on sure high-cost medical provides, and broaden billing choices for administration of behavioral well being situations in main care settings. Additional, it points requests for data (RFIs) on a number of subjects, equivalent to methods to deal with sure social and way of life elements that contribute to persistent illness, and proposes a brand new Ambulatory Specialty Model (ASM), a value-based cost mannequin for outpatient persistent illness administration. Whereas these provisions haven’t but been finalized, they supply some perception into the coverage priorities of CMS below the Trump administration. The ultimate rule can be issued later in 2025, and its provisions can be included and mentioned extra totally in future updates to this transient.
This challenge transient solutions key questions on how Medicare pays physicians and different clinicians, and critiques coverage choices below dialogue to reform this cost system. The transient is concentrated totally on the doctor cost system utilized in conventional Medicare. Medicare Benefit plans have flexibility to pay suppliers in a different way and presently there is no such thing as a systematic publicly-available data on how a lot Medicare Benefit plans pay suppliers. (See Appendix for a glossary of related packages, laws, and phrases.)
1. What’s the Medicare Doctor Price Schedule?
Medicare reimburses physicians and different clinicians based mostly on the physician fee schedule, which assigns cost charges for greater than 10,000 health care services, equivalent to workplace visits, diagnostic procedures, or surgical procedures. For providers supplied to conventional Medicare beneficiaries, Medicare sometimes pays the supplier 80% of the price schedule quantity, whereas the beneficiary is chargeable for a coinsurance of 20%. Physicians who take part in Medicare agree to just accept this association as cost in full (generally known as accepting “task”) for all Medicare coated providers. Non-participating physicians obtain 5% decrease Medicare funds, however might settle for “task” on a claim-by-claim foundation and should select to invoice beneficiaries for bigger quantities by charging further coinsurance, as much as 15% greater than the Medicare-approved quantity for the price of a coated service. A third group of physicians decide out of the Medicare program altogether, and as an alternative enter into personal contracts with their Medicare sufferers, are usually not restricted to charging price schedule quantities, and don’t obtain any reimbursement from Medicare. Only one % of all non-pediatric physicians opted out of the Medicare program in 2024.
Doctor price schedule charges for a given service are based mostly on a weighted sum of three parts: (1) clinician work, (2) observe bills, and (3) skilled legal responsibility insurance coverage (often known as medical malpractice insurance coverage). These three parts are measured when it comes to “relative worth models” (RVUs). Collectively these three parts signify the general value and energy related to a given service, with extra pricey or time-intensive providers receiving the next weighted sum. Every element is adjusted to account for geographic variations in enter prices, and the result’s multiplied by the price schedule conversion factor (an yearly adjusted scaling issue that converts numerical RVUs into cost quantities in {dollars}). Price schedule providers are every related to a singular service code, which permits clinicians to hunt reimbursement for the care they supply on a service-by-service foundation.
Cost charges specified below the doctor price schedule set up a baseline quantity that Medicare pays for a given service, however funds could also be adjusted based mostly on different elements, equivalent to the positioning of service, the kind of clinician offering the service, and whether or not the service was supplied in a delegated health professional shortage area. Physicians can even obtain quality-based cost changes below the Quality Payment Program (QPP) (see query 7).
2. How Does Medicare Replace Doctor Cost Charges?
Annual updates to the doctor price schedule embody statutorily-required updates to the conversion issue below the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) (see query 6), in addition to different changes to replicate the addition of recent providers, modifications in enter prices for current providers, and different elements. Included in these changes are periodic modifications to the RVUs assigned to price schedule service codes, based mostly partly on the suggestions of a multispecialty committee of physicians and different professionals, generally known as the AMA/Specialty Society RVS Update Committee (RUC) (see query 3).
Beneath present legislation, the projected value of all modifications to the doctor price schedule have to be price range impartial. That’s, the modifications might not increase complete Medicare spending by greater than $20 million in a given yr. This requirement was established by the Omnibus Budget Reconciliation Act of 1989 to deal with considerations that constraints on doctor charges for particular providers would result in will increase in service quantity and development in Medicare spending for doctor providers over time. The legislation requires CMS to regulate price schedule spending when projected prices exceed the $20 million threshold, sometimes by reducing the conversion issue relative to the statutory replace referred to as for by MACRA.
3. What’s the Function of the RUC in Figuring out Doctor Cost Charges?
The AMA/Specialty Society RVS Replace Committee (RUC) is a volunteer committee of physicians and different professionals, formed by the American Medical Association (AMA) in 1991 to advise CMS on the relative weighting of service codes below the doctor price schedule, the first mechanism utilized by CMS to set relative funds for doctor and scientific providers. The RUC is an unbiased physique and its operations are usually not straight overseen by Congress or CMS. Additional, as a result of the RUC will not be an official federal advisory committee, it’s not certain by federal standards round transparency, membership stability, and different working necessities utilized to many related committees. The RUC includes representatives from the AMA and different skilled organizations, in addition to members appointed by a variety of nationwide medical specialty societies.
Annually, CMS identifies doubtlessly misvalued providers for RUC evaluate based mostly on statutory standards and public nomination. Doubtlessly misvalued providers might also be recognized by the RUC itself, whereas new or not too long ago revised service codes are recognized by a separate AMA panel, generally known as the Current Procedural Terminology (CPT) Editorial Panel. The RUC then consults with varied medical specialty societies, who resolve which providers they want to evaluate and develop suggestions on the clinician work, observe bills, and different elements related to cost for every service. A remaining listing of suggestions for reviewed providers is compiled by the RUC based mostly on a committee vote and referred to CMS.
CMS will not be required to undertake suggestions issued by the RUC, nevertheless it does so in a majority of instances. The AMA studies a median annual acceptance charge of 90% from 1993 to 2025. Over time, MedPAC and others have raised considerations concerning the affect of the RUC, which is basically composed of specialty physicians with a monetary stake within the suggestions they’re producing, and famous a number of methodological points with the info used to develop RUC suggestions (see query 8). MedPAC has referred to as for CMS to develop internal processes to validate RUC suggestions by unbiased means. Extra not too long ago, HHS Secretary Kennedy has raised concerns concerning the lack of transparency and relative lack of oversight of RUC operations by CMS, in addition to the affect of the AMA in setting cost charges for physicians, which has introduced renewed attention to the problem (see query 9).
4. How Have Doctor Cost Charges Modified in 2025?
CMS recently finalized cost modifications for 2025, which embody a 2.83% lower to the doctor price schedule conversion issue relative to 2024. This lower displays the next changes: (1) the expiration of non permanent funds permitted by Congress below the Consolidated Appropriations Act of 2024, which elevated funds by 2.93% for all price schedule providers furnished between March 9, 2024 and December 31, 2024, (2) a 0% statutory enhance for 2025 below the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), and (3) a modest 0.02% price range neutrality adjustment. The mixed impression of those changes is a 2.93% lower in common funds to physicians and different clinicians, which went into impact on January 1, 2025.
As of March 2025, Congress has not handed laws to deal with this cost minimize. A provision to scale back (although not totally get rid of) the minimize was included in an early version of the year-end Persevering with Decision (CR) filed in December 2024, just like the non permanent cost changes instituted by Congress in prior years, however was faraway from the version signed into law. Congress additionally thought-about, however did not include, laws within the subsequent CR enacted in March 2025, however some policymakers proceed to push for a fix, which is reportedly into account for inclusion in an upcoming price range reconciliation invoice.
Current modifications to the doctor price schedule additionally embody a number of measures designed to enhance well being care entry and enhance help for preventive providers, behavioral well being, and administration of persistent illness. These measures are part of an ongoing effort by CMS and the Division of Well being and Human Providers (HHS) to strengthen main and preventive care and deal with long-standing concerns concerning the hole in compensation between main and specialty care physicians (see query 8). The final payment rule for 2025 introduces the next key modifications:
- CMS has added new billing codes to the doctor price schedule meant to streamline cost for advanced primary care management. This variation bundles a number of current providers associated to care administration, interprofessional session, and different care parts into single codes, stratified by affected person medical and social complexity, which can be billed on a month-to-month foundation.
- CMS has added new billing codes associated to caregiver coaching for direct care providers and helps, permitting clinicians to invoice for time spent coaching caregivers on particular scientific abilities equivalent to strategies to forestall ulcer formation, wound dressing modifications, and an infection management, and has expanded current billing choices for trainings devoted to caregiver conduct administration and modification.
- CMS has finalized a number of provisions aimed toward bettering beneficiary entry to telehealth, equivalent to broader protection of audio-only providers and elevated flexibility in the usage of telehealth for therapy of opioid use dysfunction (OUD). Security planning interventions and PrEP counseling have been added to the Medicare Telehealth Services list on a everlasting foundation, and caregiver coaching providers have been added on a provisional foundation.
- Many different telehealth restrictions that had been in place previous to the COVID-19 pandemic have not too long ago come again into impact, following the expiration of Medicare’s expanded telehealth protection pursuant to the federal government shutdown that started on October 1, 2025. These include restrictions limiting telehealth protection to beneficiaries in rural areas, and requiring beneficiaries to journey to an permitted website, such a clinic or physician’s workplace, when receiving telehealth providers. Nonetheless, CMS has prolonged sure restricted flexibilities below its authority by December 2025, equivalent to provisions that permit Rural Health Centers (RHCs) and Federally Qualified Health Centers (FQHCs) to function distant website suppliers for all coated telehealth providers, and permit suppliers to make use of their presently enrolled observe location instead of their dwelling deal with when offering telehealth providers from dwelling.
- CMS has additionally added new billing codes for a variety of different main and behavioral well being providers, equivalent to cardiovascular danger evaluation and care administration, use of digital psychological well being therapy units, and security planning interventions for sufferers liable to suicide or overdose, amongst others.
- CMS has finalized a number of updates to the Quality Payment Program (QPP) to enhance the accuracy of high quality reporting and cut back administrative burden for suppliers collaborating within the Merit-based Incentive Payment System (MIPS). (For a extra detailed description of the QPP and MIPS, see query 7).
The brand new guidelines additionally embody updates to the Medicare Shared Savings Program (MSSP), a everlasting accountable care organization (ACO) program in conventional Medicare that gives monetary incentives to suppliers for assembly financial savings targets and high quality objectives, as well as other changes related to payment for preventive vaccine administration, opioid treatment programs, evaluation and management of infectious diseases in hospital inpatient or observation settings, and a variety of other health services.
6. How Have Medicare Payments to Physicians Changed Since the Implementation of MACRA?
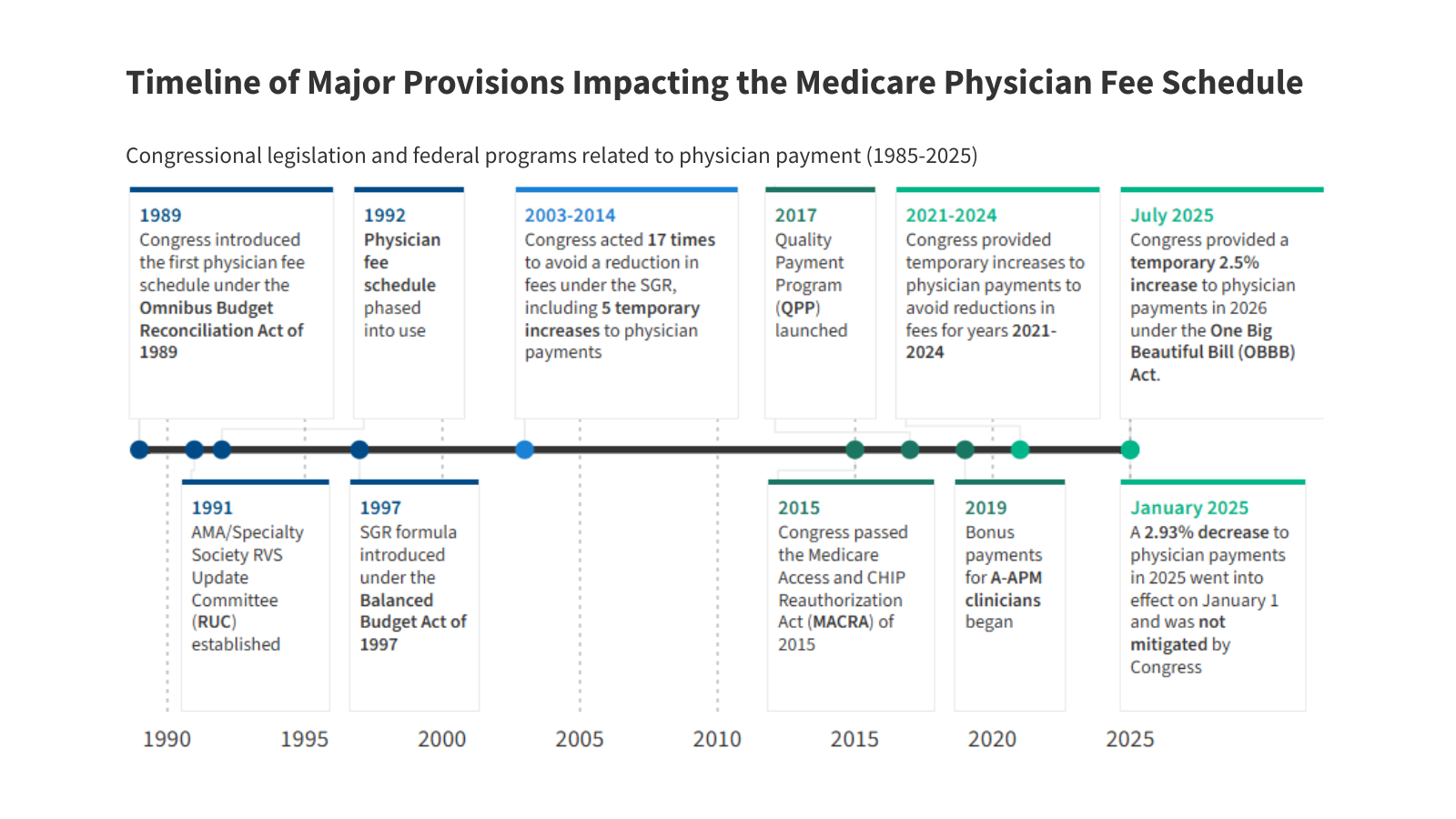
Medicare has revised its system of payment for physician services numerous times over the years (Figure 1). The current payment system was established under the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) and consists of two main parts: (1) a schedule for annual, statutorily-defined updates to the conversion issue, a key determinant of cost charges below the doctor price schedule, and (2) a brand new system of bonus funds and quality-based cost changes below Quality Payment Program (QPP) (see query 7).
The doctor cost system established by MACRA was meant to stabilize fluctuations in cost attributable to the prior system below the Medicare Sustainable Growth Rate (SGR) formula, which set annual targets for Medicare doctor spending based mostly on development within the gross home product (GDP). Beneath the SGR, if doctor spending exceeded its goal in a given yr, cost charges could be minimize the next yr, whereas spending that was under the goal led to elevated charges. As with the present system, charges had been topic to additional adjustment for price range neutrality if the projected value of all price schedule spending was projected to extend by greater than $20 million for the yr.
The SGR was established by the Balanced Budget Act of 1997 to sluggish the expansion in Medicare spending for doctor providers, however the system garnered criticism, as development in service quantity and rising prices led to a number of years of spending on doctor providers that exceeded the expansion goal, necessitating cost cuts from 2002 onward. Between 2002 and 2015, Congress enacted 17 short-term interventions (so-called “doc-fixes”) to delay the cuts and supply non permanent will increase to doctor funds, however did so with out repealing the SGR, which resulted in amassed deficits over time.
MACRA permanently eliminated the SGR system, stopping a 21.2% minimize in doctor charges slated for 2015 and changing it with 0% statutory will increase to the conversion issue by 2025 (later raised to 0.5% from 2016-2019), adopted by modest annual will increase from 2026 onward. These updates are set by MACRA and don’t differ based mostly on underlying financial situations. Nonetheless, subsequent changes to protect price range neutrality and supplemental funds supplied by Congress might end in conversion issue updates which can be greater or decrease than the statutorily-required replace in a given yr.
Though MACRA has stabilized funds below the doctor price schedule to some extent relative to the years main as much as its enactment, charges have continued to fluctuate during the last decade. On account of strict price range neutrality necessities, CMS has restricted flexibility to regulate cost charges for brand spanking new or undervalued providers with out offsetting the prices elsewhere within the price schedule. This usually takes the type of price range neutrality changes to the conversion issue, equivalent to a -10.20% adjustment in 2021 and a -2.18% adjustment in 2024. Since 2021, Congress has supplied several short-term increases to price schedule charges to spice up cost in the course of the COVID-19 pandemic and to offset budget-neutrality cuts, together with a one-time 2.5% increase not too long ago enacted for 2026.
7. How Does the High quality Cost Program (QPP) Issue Into Doctor Funds?
The Quality Payment Program (QPP), which launched in 2017, was established by the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) to create monetary incentives for well being care suppliers to manage prices and enhance care high quality. The QPP consists of two distinct pathways for participation: (1) incentive funds for members in certified advanced alternative payment models (A-APMs) and (2) efficiency based mostly cost changes below the Merit-based Incentive Payment System (MIPS).
A-APM Incentive Funds: Physicians and different clinicians who take part in certified A-APMs, equivalent to choose accountable care organizations (ACOs) and others, are eligible for bonus funds in the event that they meet sure participation thresholds. A-APMs are a kind of value-based care mannequin during which the supplier bears some monetary danger for the prices of care in an outlined setting, equivalent to therapy of a selected situation or main care providers for a gaggle of beneficiaries, sometimes by sharing in a portion of economic financial savings and losses relative to a benchmark. Incentive funds to extend participation in A-APMs are a part of a broader goal by CMS to have all conventional Medicare beneficiaries in some kind of accountable care relationship by 2030.
Annually, A-APM clinicians qualify for bonus funds based mostly on their participation in the course of the Qualifying APM Participant Performance Period (January 1 – August 31) two years prior. Beneath MACRA, qualifying A-APM clinicians acquired a 5% bonus in cost years 2019 by 2024 (efficiency durations 2017 – 2022). Congress subsequently prolonged these bonus funds to incorporate a 3.5% bonus in 2025 and a 1.88% bonus in 2026. A-APM bonus funds are scheduled to be phased out in favor of annual 0.75% will increase to the conversion issue for qualifying A-APM clinicians (relative to smaller 0.25% will increase for all different clinicians). These conversion issue updates will start in 2026, and A-APM bonus funds can be totally retired in 2027.
Roughly 386,000 clinicians certified for A-APM bonuses in 2024, based mostly on the 2022 efficiency interval, a virtually fourfold enhance from 99,000 in 2019, the primary yr A-APM bonuses had been obtainable. On the similar time, A-APMs are not evenly distributed all through the nation, and participation amongst non-physician suppliers and sure doctor specialties remains relatively low, suggesting that further methods could also be wanted to encourage wider adoption of those fashions. Additional, MedPAC and others have famous that the scheduled conversion issue updates for qualifying A-APM clinicians can be comparatively small within the first few years after A-APM bonuses are retired, although their results will compound over time, and have cautioned that further incentives could also be wanted to forestall attrition in A-APM participation throughout this transition.
Advantage-based Incentive Cost System (MIPS): Clinicians who don’t take part in A-APMs, or don’t meet the participation standards for A-APM bonus funds, are topic to further reporting necessities below MIPS, which adjusts funds up or down relying on a clinician’s efficiency on sure high quality metrics. As with A-APM bonuses, cost changes below MIPS are based mostly on efficiency two years prior. Clinicians are required to take part in MIPS if they’re eligible, however many are exempt, equivalent to these in sure specialties (e.g., podiatrists), these of their first yr of Medicare participation, and people who serve a low quantity of Medicare sufferers.
Cost changes below MIPS are required to be price range impartial. Changes are capped annually (between +9% and -9% in 2025), and financial savings generated from clinicians who incur damaging changes are used to fund optimistic changes for many who qualify. As a result of a relatively small share of clinicians have incurred damaging changes annually since MIPS was carried out, optimistic changes have typically been a lot decrease than the annual cap. In 2023 for example, roughly 600,000 clinicians acquired optimistic changes as much as +2.34%, based mostly on the 2021 performance year, whereas simply 23,000 clinicians acquired damaging changes right down to -9%. MedPAC estimates that another 460,000 clinicians had been ineligible for both an A-APM bonus or MIPS adjustment because of low Medicare affected person quantity or different exemption standards.
Clinicians who take part in MIPS have historically selected from a large set of high quality measures and different scientific metrics to report on annually. Whereas this construction was meant to provide clinicians flexibility to decide on the metrics finest suited to their observe, it has additionally been criticized by physician groups and experts for growing the reporting burden on members, and for making comparisons between members much less clinically significant and harder to evaluate. In an effort to deal with these considerations, CMS has launched a number of extra streamlined reporting options. The latest of those permits clinicians to select from smaller, bundled subsets of reporting metrics tailor-made to explicit specialties or medical situations, generally known as MIPS Value Pathways (MVPs).
MVPs had been launched in 2023 as an non-obligatory different to reporting below conventional MIPS, and included a preliminary set of reporting pathways aimed toward particular scientific contexts, equivalent to main care, therapy of coronary heart illness, and supportive look after neurodegenerative situations. CMS has added new MVPs annually for the reason that choice was launched, including 6 in 2025, with the eventual goal of changing all reporting below conventional MIPS with MVPs in future years. The purpose of this shift is to scale back administrative burden by providing suppliers smaller, extra focused units of reporting metrics to select from, in addition to to permit for extra clinically significant assessments by evaluating outcomes amongst related clinicians who select to report below the identical MVP.
8. What Considerations Have Been Raised In regards to the Doctor Price Schedule?
Criticism of the doctor price schedule has centered on 4 main considerations about the way in which during which Medicare pays physicians and different clinicians. These embody: (1) the general adequacy of Medicare funds to cowl medical observe prices and incentivize participation within the Medicare program, (2) the hole in compensation between main and specialty care clinicians, (3) the affect of the AMA/RVS Update Committee (RUC) and medical specialty teams in figuring out relative cost charges for price schedule providers, and (4) the success of the Quality Payment Program (QPP) in attaining its objective of incentivizing high quality enhancements and cost-efficient spending.
Cost Adequacy: Over time, physician groups and some policymakers have expressed concern that cost charges below the doctor price schedule have not kept pace with inflation in medical observe prices. Observe bills are one element of the relative-value calculation used to find out cost charges for price schedule providers, however the requirement to protect price range neutrality makes it troublesome for CMS to extend cost for some providers with out additionally reducing cost in different areas, equivalent to by decreasing the price schedule conversion issue (see query 6). Statutory will increase to the conversion issue below MACRA are usually not scheduled to start till 2026, and don’t differ based mostly on underlying financial situations, which can make it more difficult for some physicians to adapt to altering monetary calls for.
Core to those considerations is the likelihood that lack of revenues could lead on some physicians to decide out of the Medicare program, which might create access issues for Medicare beneficiaries. Nationwide surveys and different analyses have typically discovered that beneficiaries report entry to doctor providers that’s equal to, or better than, that of privately-insured people, with related or smaller shares reporting delays in needed care or difficulty finding a physician who takes their insurance. A recent KFF analysis discovered that simply 1% of all non-pediatric physicians had opted out of Medicare in 2024, suggesting that the present price construction has not considerably discouraged participation. Furthermore, MedPAC estimates that virtually all Medicare claims (99.7% in 2023) are accepted on “task” and paid at the usual charge (see query 1), with beneficiaries in conventional Medicare going through not more than the usual 20% coinsurance charge. On the similar time, analyses by KFF and others have discovered that physicians in some specialties, equivalent to psychiatry, decide out of Medicare at greater charges, which can impression entry to those providers over time.
Lack of income might also lead some doctor practices to merge with (or be acquired by) bigger well being methods or hospitals, a course of generally known as “vertical consolidation.” Vertical consolidation might supply certain benefits to physicians, equivalent to better financial system of scale for observe bills, decrease administrative burden, and entry to pricey sources equivalent to medical imaging gear, and could also be enticing to physicians who’re in any other case struggling to satisfy their observe prices. Whereas consolidation could also be related to some benefits to patients as nicely, equivalent to enhancements in care integration and coordination between suppliers, it might additionally result in greater out-of-pocket prices and decrease care high quality by reducing market competition. Additional, Medicare typically pays more for a given service supplied in a hospital outpatient division than it does for a similar service supplied in a freestanding doctor workplace, which may result in elevated prices for beneficiaries and better program spending over time. Policymakers are presently exploring choices to align Medicare reimbursement charges between these settings, generally known as “site-neutral payment reforms.”
Major Care Compensation: A second concern with the present cost system is that Medicare doesn’t adequately pay for main care providers, as mirrored by the gap in Medicare payments between main and specialty care clinicians. Funds below the doctor price schedule are typically greater for scientific procedures, equivalent to surgical procedures and diagnostic exams, than for non-procedural providers, equivalent to preventive care supplied throughout an workplace go to. Whereas many clinicians present a combination of procedural and non-procedural providers, main care clinicians usually dedicate a larger share of their time to non-procedural care. Additional, MedPAC has expressed concern that this imbalance encourages clinicians of all specialties to increase their use of extra pricey and worthwhile providers, equivalent to pointless imaging, screenings, and diagnostic exams, on the expense of high-value, however much less worthwhile, providers, equivalent to affected person schooling, preventive care, and coordination throughout care groups, which may impression the standard of affected person care and result in greater doctor spending over time.
MedPAC notes that scientific procedures usually see gains in efficiency because of technological enhancements and different elements, which cut back the effort and time wanted to offer them. If price schedule charges are usually not adjusted to replicate these enhancements, these providers might turn out to be overvalued over time. In contrast, non-procedural providers usually contain extra fastened time constraints, equivalent to time spent speaking with sufferers or coordinating with different suppliers, and are unlikely to see related positive aspects, contributing to the hole in compensation between these service sorts.
On account of price range neutrality necessities, efforts to straight enhance cost for non-procedural providers below the doctor price schedule with the intention to increase funds for main care have usually necessitated across-the-board cost cuts within the type of decreases to the fee schedule conversion factor (see query 6). Additional, physicians might offset any anticipated reductions in income by increasing service volume over time, or by increasing their use of upper depth, and extra extremely compensated, service codes, leaving the hole in cost charges comparatively fixed. These constraints make it troublesome for CMS to meaningfully deal with variations in cost between main and specialty care, and have led some policymakers to voice considerations that the present price range neutrality necessities are too inflexible.
Function of the RUC: The American Medical Affiliation (AMA) and the RUC play a considerable position in annual decision-making across the relative weighting of service codes below the doctor price schedule, the first mechanism utilized by CMS to set relative cost charges for doctor and scientific providers (see query 3). Whereas CMS will not be required to undertake suggestions issued by the RUC, it does so in a majority of cases. MedPAC has raised a number of methodological concerns with the info utilized by the RUC to develop its annual studies, that are largely based on recommendations from medical specialty societies. These embody a scarcity of transparency, in addition to low response charges and complete responses on the varied member surveys that inform medical specialty society suggestions, which make it troublesome for CMS to validate RUC suggestions by different means.
Different considerations raised concerning the RUC embody the overrepresentation of specialty physicians on the committee, and the potential for conflicts of curiosity when RUC members advocate modifications to relative funds for main and specialty care providers. In distinction to federal advisory committees, that are sometimes shaped by Congress, the workplace of the President, or govt department companies, the RUC is an unbiased committee overseen by the AMA. For that reason, it’s not held to the identical operating requirements as many different related committees, which adhere to sure standards round transparency and membership stability. The Secretary of the Division of Well being and Human Providers (HHS), Robert F. Kennedy Jr., has echoed many of those considerations in current months, and has referred to as for bringing greater transparency to the operations of the RUC (see query 3), in addition to exploring options for decreasing the position the RUC performs in annual decision-making round doctor funds.
To make sure that price schedule providers are usually not overvalued, MedPAC has recommended that CMS develop inner processes for validating RUC suggestions, equivalent to by gathering information from scientific practices on the variety of clinician hours devoted to commonly-billed providers. Pilot research commissioned by CMS and the Division of Well being and Human Providers (HHS) have attempted to validate the clinician time element of small subsets of price schedule providers utilizing strategies equivalent to evaluation of digital well being information, direct commentary of scientific procedures, and independently-collected doctor surveys. These tasks might function a blueprint for future work, although implementing these and related strategies on a big scale would possible require important time and employees funding.
Function of the QPP: QPP packages equivalent to the Merit-based Incentive Payment System (MIPS) and bonus funds for Superior Different Cost Mannequin (A-APM) clinicians are designed to create incentives for high quality enchancment, care coordination, and the supply of high-value providers (see query 7). Whereas the share of clinicians who qualify for A-APM bonuses has greater than tripled for the reason that QPP started (from roughly 99,000 to 386,000 within the 2017 and 2022 efficiency durations, respectively), some policymakers have argued that better incentives are wanted to encourage suppliers to tackle the monetary dangers and excessive startup prices related to these fashions, significantly as A-APM bonus funds are phased out in favor of comparatively smaller conversion issue changes within the coming years.
Moreover, MedPAC has voiced concern that MIPS, the quality-based cost program for clinicians who don’t take part in A-APMs, imposes too giant of a reporting burden on those that take part, whereas on the similar time providing comparatively weak incentives to enhance high quality and management prices. As famous earlier, a large share of clinicians are exempt from this system, and since few members obtain damaging changes, optimistic changes are relatively modest. The executive burdens related to MIPS could also be partially addressed by the shift in the direction of MIPS Value Pathways (MVPs) instead of conventional high quality reporting, and additional evaluation of this feature will possible take form as this system is phased in.
9. What Coverage Proposals Have Been Put Ahead to Deal with Considerations with Medicare’s Present Doctor Cost System?
Along with recent legislation that gives a short lived 2.5% enhance to doctor cost charges in 2026, policymakers and others have put ahead quite a lot of methods to revise the present Medicare doctor cost system. These embody measures to stabilize doctor price schedule funds from yr to yr, present further help to main care and safety-net suppliers, and create stronger incentives for environment friendly spending, care coordination, and participation in Superior Different Cost Fashions (A-APMs).
In 2025, MedPAC recommended a one-time inflation-based enhance to doctor cost charges in 2026 (equal to the projected enhance within the Medicare Financial Index minus one share level), just like suggestions from past years. Whereas MedPAC has weighed the possibility of recommending annual updates for inflation, it has not carried out so so far, focusing as an alternative on focused methods to bolster funds to main care clinicians and safety-net suppliers. As an example, in gentle of findings that clinicians usually obtain decrease income for treating low-income Medicare beneficiaries, MedPAC has advisable elevating cost in these instances by 15% for claims billed by main care clinicians and 5% for claims billed by non-primary care clinicians, to encourage clinicians to deal with these populations.
MedPAC has voiced help for the objectives behind the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) and the Quality Payment Program (QPP), together with the monetary incentives supplied to A-APM members below present legislation (see query 7), whereas additionally recommending changes to the design of the QPP, together with the elimination of the Merit-based Incentive Payment System (MIPS). MedPAC has noted that the continuing shift from conventional MIPS to MIPS Value Pathways (MVPs) addresses some considerations associated to administrative complexity and participant comparisons, however a big share of clinicians stay exempt from MIPS reporting and incentive funds have typically remained comparatively small (see query 8). Instead of MIPS, MedPAC has advisable establishing a voluntary program designed to imitate the construction of A-APMs and different alternative payment models, permitting clinicians to transition into these fashions extra progressively.
A number of payments launched within the final Congress point out curiosity in methods such elevating or modifying the price range neutrality threshold, or providing separate conversion issue updates for main and specialty care providers, which might permit CMS better flexibility to regulate cost charges to replicate evolving coverage priorities with out necessitating a compulsory cost minimize. The Senate Finance Committee has held a number of hearings on doctor price schedule reform, and launched a whitepaper in 2024 outlining a variety of choices to stabilize conversion factor updates from yr to yr, extend access to telehealth, and incentivize continued participation in A-APMs, amongst different reforms.
Extra not too long ago, CMS has proposed rulemaking changes for doctor funds in 2026, which embody potential changes to the relative value calculations used to tell cost charges for price schedule providers. Particularly, CMS has proposed to complement information and suggestions from the AMA and the RUC with information from further sources, such because the Medicare Hospital Outpatient Prospective Payment System and the Medicare Financial Index productiveness adjustment, when calculating sure points of doctor work and observe expense RVUs. Whereas these modifications haven’t but been finalized, they’re in step with objectives voiced by HHS Secretary Robert Kennedy Jr. to promote independence from the RUC, and counsel that CMS has an curiosity in growing methods for inner code evaluate.
A decade after the passage of MACRA, Congress’s final main overhaul of how Medicare pays physicians, curiosity in broader reforms to Medicare’s doctor cost system, is gaining steam. Designing cost approaches that deal with considerations raised by events to compensate physicians adequately whereas restraining spending development represents a problem for policymakers.
This work was supported partly by Arnold Ventures. KFF maintains full editorial management over all of its coverage evaluation, polling, and journalism actions.